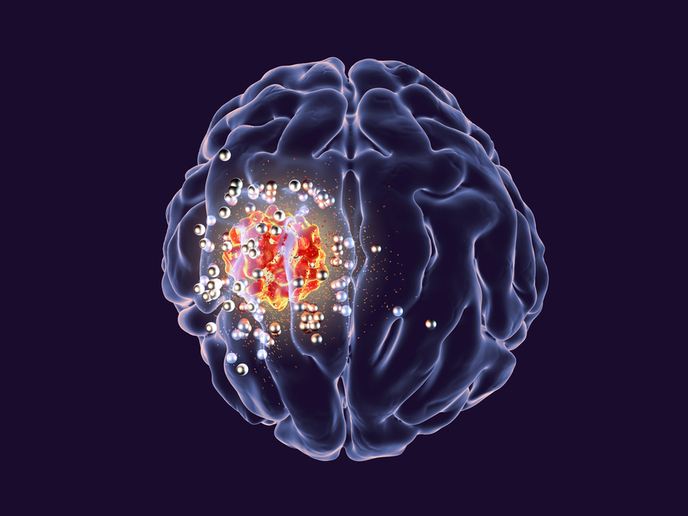
Nanoparticles deliver drugs directly to the brain
Brain tumours are difficult to treat because of their invasive nature and aggressiveness. Another major obstacle is the natural protection of the brain that separates it from the systemic circulation, posing a challenge to treatment with systemic drugs.
A polymer-based approach for drug delivery
Undertaken with the support of the Marie Skłodowska-Curie programme, the HyGlio project addressed drug delivery to the brain and imaging through the development of a multifunctional polymer-based tool that combines hydrogels and nanoparticles. “By combining hydrogels and nanoparticles, we can merge the advantage of long-term release from hydrogels and the targeting ability of nanoparticles, in the hope of extending residence time of drugs in the tumour area,” explains the Marie Skłodowska-Curie fellow Clara Mattu. HyGlio was a collaboration between the Polytechnic University of Turin and the Houston Methodist Research Institute in the United States, where the fellow spent 2 years as part of the outgoing phase of the project. When designing particles for drug delivery, scientists must take into account the surface properties of the nanoparticle carriers as they will determine cell interaction, in vivo biodistribution and tumour accumulation. In this context, the research fellow employed polyurethane-based nanoparticles 100-200 nm in diameter to load drugs. These nanoparticles contained both hydrophobic and hydrophilic domains that enhanced the affinity for both hydrophilic and hydrophobic drugs and showed an overall improvement in biodistribution and half-life within the body. Moreover, the fellow combined nanoparticles with hydrogels that are suitable for localised drug delivery and facilitate slow release. The use of thermo-responsive hydrogels ensured that the gel is liquid and injectable at room temperature and quickly forms a 3D network when it reaches body temperature at the place of injection. To study the tumour, Mattu loaded nanoparticles with fluorescent markers or other imaging probes that allow magnetic resonance imaging. “We, and others, have shown that concomitant loading of drugs and imaging probes can be achieved within nanoparticles,” she emphasises.
Efficacy of the hydrogel drug delivery approach
Although the approach is in the early stages of development, preliminary in vivo data suggest that the combination of hydrogels and nanoparticles is safe and, most importantly, that nanoparticles can reside in the brain and in the proximity of the tumour for longer. Tumour-bearing experimental animals retained drug-loaded nanoparticles for up to 10 days post intra-tumoural injection, and the drug exhibited good biodistribution in the tumour and improved the animals’ survival. Moreover, scientists observed modifications in the number and structure of tumour blood vessels after treatment. Future plans include the testing of drug combinations in dual release strategies, where drugs are loaded partly in nanoparticles and partly in the hydrogel compartment. Cancer therapy often requires the concerted and combined action of different chemotherapeutics to overcome drug resistance and improve patient outcome. However, synergistic treatment is hampered by incompatible pharmacokinetics and hydrophobicity of the different drugs. HyGlio proposes to overcome this through the combination of hydrogel with polyurethane nanoparticles for efficient encapsulation of both hydrophobic and hydrophilic drugs, achieving maximal tumour accumulation and treatment efficacy.
Keywords
HyGlio, drug, nanoparticle, hydrogel, drug delivery, biodistribution, brain tumour, polyurethane