Advancing therapeutic applications of gene editing
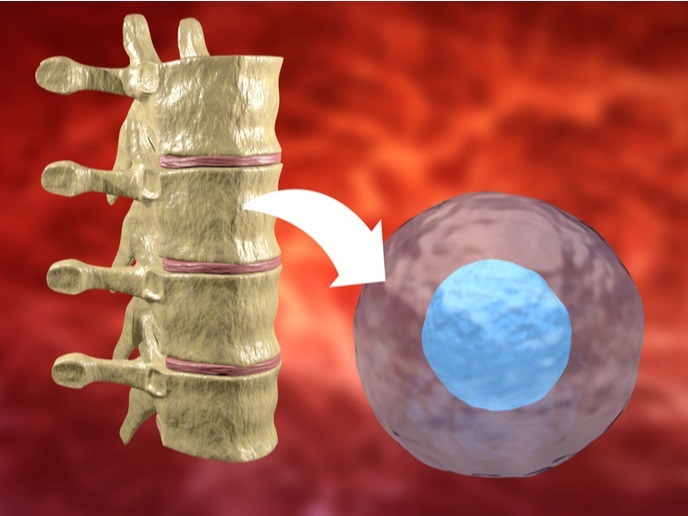
The idea of defective gene replacement has long been envisioned for many debilitating or fatal diseases. For inherited haematological or immune disorders, genetically modified hematopoietic stem cells (HSCs) are an ideal means of providing long-term correction given the capacity of these cells to self-renew and to differentiate into a diverse range of specialised cell types. In addition, autologous transplantation of corrected HSCs essentially overcomes the immunological complications of graft rejection and post-transplant immunosuppressive therapy. Preclinical evidence alongside initial clinical trials support the safety and benefits of HSC-based gene therapy. However, the use of semi randomly integrating vectors might still cause adverse consequences such as insertional mutagenesis and unregulated or ectopic transgene expression. These may in turn lead to oncogenesis or elimination of the modified cells, jeopardising the efficacy of the approach. The EU-funded SUPERSIST (Towards clinical translation of new gene targeting technologies for correcting inherited mutations and empowering adoptive immunotherapy of cancer) project wished to overcome these limitations by employing innovative key technologies for ex vivo gene targeting. The project came as a continuation of the successful European initiative PERSIST which delivered advanced HSC gene delivery methods for the safe and effective gene therapy of a range of human diseases. Endogenous correction of the defective gene Intriguingly, the SUPERSIST approach aimed to trigger the endogenous cell repair mechanisms to correct or inactivate the mutated gene. To this end, researchers utilised endonucleases, such as zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) engineered to recognise and cut the mutated gene, awakening the homologous recombination mechanism. The enzymes were transiently delivered ex vivo to HSCs together with a template for the desired edit and the targeted gene was successfully modified to the new version. As explained by the consortium, ‘The approach undertaken has the advantage to restore the function of the gene as well as its physiological expression control. In addition, most disease-causing mutations affecting the genetic locus, including deletions, can be treated with the same engineered nucleases.’ The therapeutic potential of the SUPERIST genome-editing strategy was demonstrated by targeting the common gamma chain receptor (IL2RG) gene, a key component of many interleukin receptors involved in immune system function, which is defective in a severe form of primary immunodeficiency. When gene-edited HSCs were transplanted in mice, they sustained normal haematopoiesis and gave rise to functional lymphoid cells. Immunotherapy for cancer Over the years, gene therapy has expanded its potential applications to encompass cancer treatment, mainly by activating anti-cancer immune responses. One of the strategies aims to genetically engineer T cells to kill cancer cells by transferring cancer-specific T cell receptors (TCRs) that recognise cancer antigens. However, the approach was met with limited clinical efficacy possibly due to competition with endogenous TCRs, thus increasing the risk of generating unpredictable new specificity by mismatching the exogenous and endogenous TCR chains. ‘To overcome these hurdles, the SUPERSIST consortium performed simultaneous knockout of the endogenous and introduction of tumour-specific TCR genes’ notes project coordinator Professor Naldini. In view of the clinical translation of the approach, they optimised the protocol and tested its validity in preclinical models. Upon infusion into tumour-bearing mice, the gene-edited T cells safely cleared the tumour without producing adverse effects and presented an early memory T cell phenotype that supported their long-term persistence following transplantation. Partners further envision that ‘with the support of their SME partners they will be able to scale-up the optimised gene targeting protocols for clinical testing.’ Overall, SUPERSIST results for a targeted gene-editing approach will lead to more precise and robust gene therapy strategies. In turn, this will extend applications beyond inherited disorders such as for adoptive T cell therapy, an approach that is gaining momentum in cancer treatment.