Pioneering nanoparticles deliver targeted cancer treatments
While the treatment of cancer remains a critical healthcare challenge, new anticancer drugs are continually being developed. However, selectively killing cancer cells while reducing damage to healthy cells remains problematic. A new weapon in this fight has been nanomedicine(opens in new window). Nanoparticles(opens in new window) loaded with anticancer drugs are continually being developed and tested, with the aim of improving drug delivery, efficacy and tolerability. Despite impressive advances however, only a relatively small number of nanomedicine products are approved for clinical use. “People often think that nanomedicines go straight to the tumour,” explains PIcelles project coordinator Twan Lammers, researcher at RWTH Aachen University(opens in new window) in Germany. “But this is not the case. Nanodrugs injected into the bloodstream need to get out of tumour blood vessels, to eventually end up near cancer cells.” As a result, many nanomedicines fail to boost response rates and survival times in patients. To improve success rates in trials, a more rational and more holistic approach is required.
Targeted drug delivery
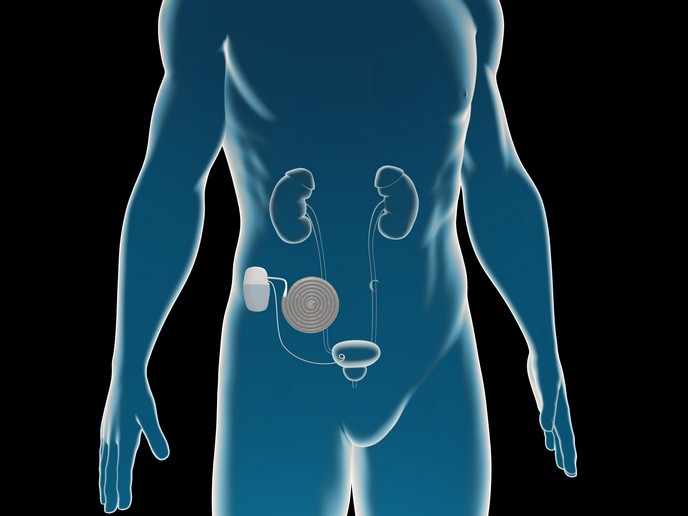
The EU-funded PIcelles project set out to achieve this goal. The project builds on previous work on non-invasive imaging, used to assess whether nanoparticles are effectively accumulating at the target site. “We recognised the importance of first being able to see whether patients are likely to be responsive to treatment,” says Lammers. The goal of PIcelles was to take this work one step further. In addition to employing non-invasive imaging to preselect patients, the project team has developed nano-sized polymeric micelles(opens in new window) that can efficiently penetrate the tumour. “Their small size, along with penetration-promoting peptides on the surface, help to improve tumour-targeted drug delivery and promote anticancer efficacy,” adds Lammers. The outer shell of polymeric micelles is hydrophilic(opens in new window), which means that it is soluble and disperses well in the bloodstream. The core is hydrophobic(opens in new window) and suitable for encapsulating potent chemotherapeutic compounds that often have very poor solubility.
Improved patient care
The success of the PIcelles project has enabled Lammers and his team to look at follow-up funding to start scaling up polymeric micelle production. To move forward towards investments and/or licensing deals with pharmaceutical industries, it is important to secure a strong patent portfolio. “This would not have been possible without ERC funding,” notes Lammers. “For academics, it is really difficult to bridge that gap between research and the market, and the first thing that investors look for is patents.” Ultimately, the breakthroughs achieved through PIcelles, and previous related https://erc.europa.eu/ (European Research Council)-funded projects, will benefit cancer patients. “Talking about quality of life, think about a woman in her mid-30s diagnosed with triple-negative breast cancer,” he says. “If there is no targeted treatment available, then she will be given a cocktail of chemotherapeutic drugs which often has numerous side effects. Along with bone marrow depression these can also include neurological toxicities, nausea and hair loss.” By encapsulating chemotherapeutic drugs into nanomedicine formulations, such as polymeric micelles, many of these side effects can be avoided, because the drug will not go to the majority of healthy tissue. “This might not be something that is always appreciated by investors, who are typically looking for radical improvements in efficacy, but it is definitely appreciated by patients,” adds Lammers. “If we could combine nanomedicine-based tolerability improvements with therapeutic efficacy enhancement, that would really be a giant leap forward for the cancer nanomedicine field.”