mRNA nanoparticles can programme cells to treat eye diseases
In Europe, the most common causes of impaired vision, or blindness in extreme cases, are age-related macular degeneration (AMD), glaucoma and diabetic macular edema (DME). AMD and DME are usually treated with protein drug injections into the eye’s vitreous cavity(opens in new window), reducing retinal edema (swelling) and slowing down disease progression. Glaucoma is treated with eyedrops to reduce pressure in the eye. “While AMD and DME treatments should be injected into the eye every one to two months, intervals are often longer, and while injections can reduce diseased ocular blood vessels’ leakiness, retinal degeneration continues. Likewise, glaucoma eyedrops don’t protect the retina and optic nerve,” says Arto Urtti(opens in new window), coordinator of the LIPOmRNA project, which was funded by the Marie Skłodowska-Curie Actions(opens in new window) programme. LIPOmRNA’s answer was to manufacture a lipid nanoparticle (LNP) holding mRNA(opens in new window) able to induce cells to produce therapeutic proteins, paving the way for new injection and eye drop treatments, as part of a wider suite of forthcoming innovations.
Programming cells to produce medicine
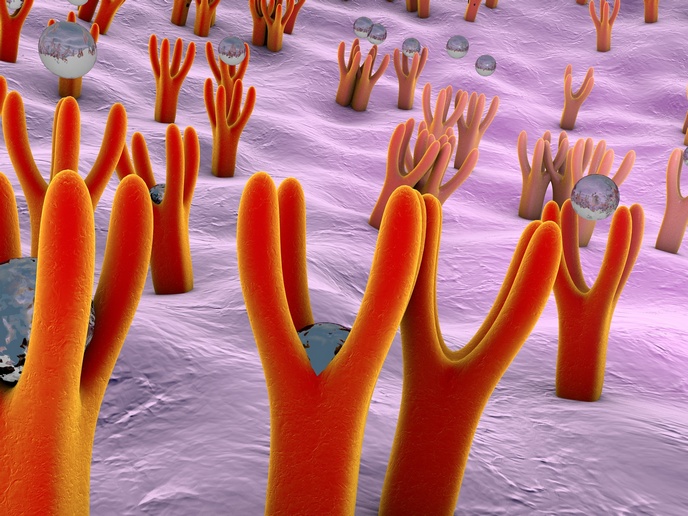
LIPOmRNA leverages the way the human body produces therapeutic proteins. Cells use mRNA to read the body’s genetic code (DNA) and produce proteins to perform many actions, including decreasing blood vessel leakiness or regenerating diseased tissue. “While proteins themselves can be used as drugs, better to use mRNA to produce therapeutic proteins in situ, effectively programming cells to manufacture medicine,” explains Urtti from the University of Eastern Finland(opens in new window), the project host. To deliver the mRNA to the target cells, virus-sized lipid-based nanoparticles were developed to bind and package mRNA. “If delivered on its own, mRNA would be degraded; even intact it couldn’t enter cells,” Urtti explains. The LNPs comprise different lipids and can be coated with other materials, such as hyaluronic acid(opens in new window) which naturally occurs in many tissues, including the vitreous. For LNPs to permeate ocular tissues, their surface must be negatively charged or neutral. They are then ‘eaten’ by target cells (endocytosis), enabling the mRNA to trigger protein production.
Testing mRNA therapeutics in cells and animal models
To understand the impact of LNP composition, different-sized nanoparticles were characterised and given to cultured retinal cells. “Interestingly, we discovered that cell uptake and protein production do not always correlate, because different LNPs can release active mRNA differently within the cells,” notes Urtti. Not yet possible to predict LNP actions through computer modelling, the most promising LNPs were tested as ocular injections in rabbits and rats, with LNP retinal distribution analysed using a method based on mass spectrometry. To reduce animal testing, a method was developed for testing 10 different LNPs in one injection. “Some LNPs entered the retina after intravitreal injection more effectively than traditional nanoparticles such as liposomes, and LNP retention was over two months – promising for long-acting injections,” adds Urtti. Some LNPs were also tested as eye drops to convert corneal cells at the eye surface into protein-producing ‘factories’, with the protein products measured in tear fluid. “Here, we got the best results using hyaluronic acid-coated LNPs, as these adhere to the ocular surface’s mucin, stopping them from being washed away. Furthermore, these LNPs seem ‘tastier’ to cell receptors,” remarks Urtti.
For more effective eye injections and topical medications
Crucially, LNP delivery by injection is not dependent on a nucleotide(opens in new window) sequence, meaning that the method could be used for any mRNA code, introducing possibilities for further retinal treatments. Meanwhile, LNP-delivered mRNA can prompt protein production on the ocular surface, also independent of mRNA code, making eye drops to treat uveitis (ocular inflammation) a possibility, currently only possible by injection. “Longer intervals between injections and topical medication delivery will help reduce the suffering of patients and the burden on healthcare services,” says Urtti.