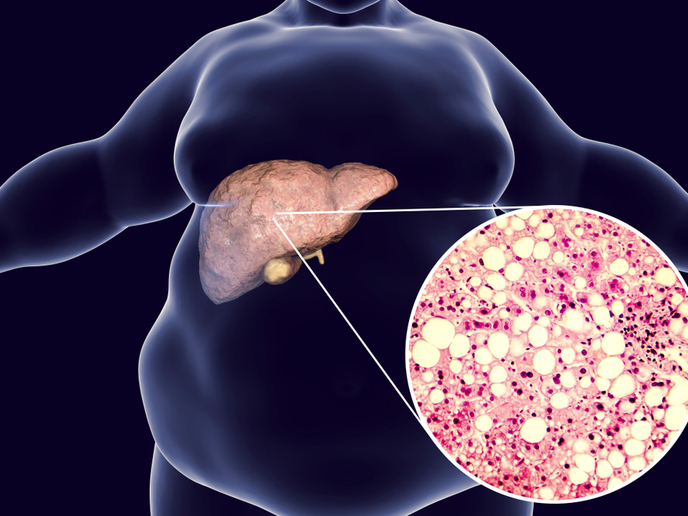
Liver-mimicking tissue as an alternative to transplants
The dramatic rise in obesity and Type 2 diabetes has led to a higher prevalence of liver-related diseases, and subsequent demand for liver transplants. Due to a shortage of liver donors, this presents a major global medical challenge. “The need is huge and the donors are too few,” says Brigitte Städler(opens in new window), a professor at Aarhus University. “Also, not every individual qualifies for the transplant list, due to poor perspective, poor life choices and so on.” To support these patients, clinicians need not synthetic livers, but liver-like devices outside of the body that support the patient over a critical phase, potentially allowing the inherent regenerative capabilities of the liver to act. In the ArtHep project, which was funded by the European Research Council(opens in new window), Städler and her colleagues developed liver-like tissue, combining both biological and synthetic parts, which mimic specific parts of the core structure and functions of the human liver. “We fabricated semi-synthetic tissues that could potentially be used in extracorporeal liver support devices, though there is still a long way to go,” Städler adds. “In parallel, we also will explore this synthetic tissue as an intermediate between 2D cell culture and liver organoids or liver slices for testing new medical interventions.”
Developing, testing, bioprinting semi-synthetic liver tissue
When developing semi-synthetic tissue, there are two aspects to consider, Städler explains. On the one hand, artificial cells must imitate a selected aspect of hepatocytes (the primary cells of the liver). On the other hand, the mammalian cells have to accept the artificial cells as they proliferate (increase in number). The researchers therefore used cell membrane vesicles originating from hepatocytes to cloak the artificial cells. “In other words, the artificial cells ‘looked’ like hepatocytes to the living mammalian cells,” Städler says. The team used 3D bioprinting to fabricate the cm-sized semi-synthetic tissue. The ink contained a liquid phase, which mostly acted as nutrition for the mammalian cells and let them remodel the environment during proliferation. The solid phase was a combination of hepatic cell aggregates and artificial cells.
Interfacing artificial with mammalian cells
When interfacing artificial cells with the living world, mammalian cells will proliferate, while the number of artificial cells doesn’t change as they do not have any self-replication capabilities – a substantial limitation. “Self-replication – which is an essential feature of life – requires division and growth cycles, which remains unaccomplished in synthetic systems,” explains Städler. “To address this challenge, we illustrated protein-mediated division of vesicles using a single membrane-modulating enzyme, unique due to its simplicity and efficacy without inherent limitations that would hamper the development of a self-replicating artificial cell.”
Building connections within the scientific community
ArtHep allowed Städler to establish strong connections with clinical hepatologists in both Aarhus and London, and she hopes they will take the basic science down the translational road, so that eventually affected individuals will benefit. The work integrating artificial and mammalian cells has already captured the attention of the scientific community. “When we started ArtHep in 2019, we were the odd ones out who tried to explore artificial cells in the context of tissue engineering, to have artificial cells integrate and communicate with mammalian cells,” notes Städler. “Today, the field is exploding, with reports on this topic fast becoming a mainstream research endeavour in bottom-up synthetic biology.”