Organ-on-chip innovation boosts biomedical research
Organoid technology involves the creation of mini organs or 3D tissue structures in a laboratory setting using stem cells. This advanced technology enables researchers to study biological processes, model diseases, discover new drugs and progress personalised medicine and regenerative therapies. “Over the last decade, several complex organ-on-chip (OoC) technologies have been developed, such as lung-on-chip, blood-brain-barrier (BBB)-on-chip and skin-on-chip,” notes GUTVIBRATIONS(opens in new window) project coordinator Katja Wolthers from Amsterdam University Medical Centre(opens in new window) in the Netherlands. “However, current OoCs available are not always user-friendly, and might not be relevant to practical applications.”
A gut-brain axis organ-on-chip
The GUTVIBRATIONS project sought to take OoCs to the next level by combining STACKS technology (a 3D-printed platform), organoid models and bio-silk (a biomaterial made from spider silk protein). The goal was to develop a gut-brain axis OoC that simulates one of the routes that connects the interaction between the gut and the brain. “This interaction is increasingly important for human health and disease,” explains Wolthers. “Our aim was to provide an innovative solution for modelling human diseases and preclinical drug development.”
Silk nanomembranes and gut epithelial cells
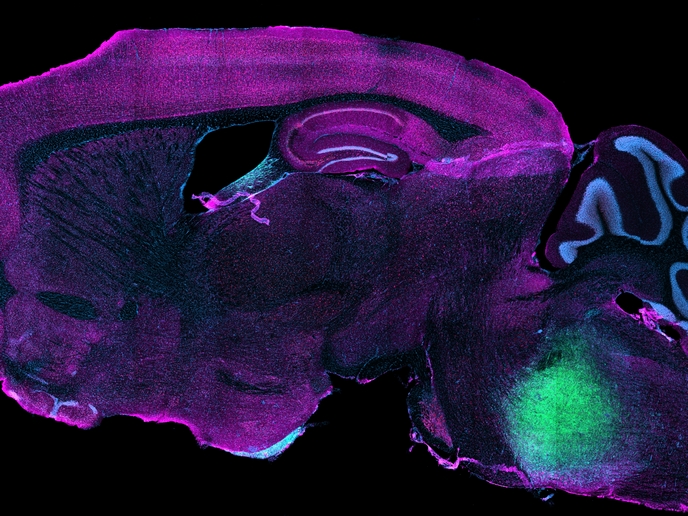
In the project, a number of new techniques were pioneered. These include the production of silk nanomembranes and the co-culture of gut epithelial cells (cells that line the gut) and fibroblasts (connecting tissue cells). Conditions to support the co-culture of intestinal epithelial cells and immune cells were also established. Induced pluripotent stem cells (iPSCs) necessary for BBB assembly – such as astrocytes, pericytes and microglia – were identified and tested. iPSCs are a type of stem cell that can be reprogrammed, enabling them to differentiate into any cell type in the body. This makes them valuable for disease modelling, drug discovery and regenerative medicine. The project team, which included industrial partners as well as academics, also designed and optimised 96-well STACKS scaffolds in which cell cultures could be contained.
Combining gut mucosa models and BBB-brain models
The project team was successful in building a number of new OoC models. These include a gut mucosa model (which replicates the structure and function of the lining of the intestine) as well as a BBB model. A gut-brain axis OoC was then built through combining the gut mucosa model and BBB-brain model. “We are currently collaborating with other European researchers to apply our model to understand the relation between viral infections and neurodegenerative diseases such as Alzheimer’s disease and Parkinson’s disease,” says Wolthers. “Our model can also be applied to study non-virus gut-brain pathology, such as the effects of inflammatory bowel disease (IBD) on the brain, and to help find drugs to counteract such effects.” Innovations pioneered in the GUTVIBRATIONS project will hopefully help to fast-track drug development that minimises animal use, lowers disease burden and ultimately saves lives. Projects such as this are also critical to maintaining Europe’s position at the cutting edge of biomedical research. “We also hope to have increased awareness and knowledge about medical regulatory policies and requirements, especially among academics and SMEs,” adds Wolthers.